Acute Pancreatitis
*Please note: This slide set represents a visual interpretation and is not intended to provide, nor substitute as, medical and/or clinical advice.
Acute pancreatitis is the sudden inflammation of the pancreas. It can be very painful and usually means a stay in the hospital. About 5% of cases are life-threatening; usually when other organs are involved.
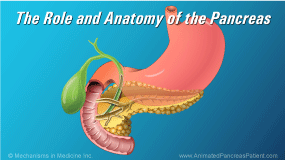
The pancreas is a digestive system organ that has two important functions. It produces enzymes to break down food in the digestive tract, as well as hormones that regulate blood sugar.
In acute pancreatitis, the enzymes used to break down food become activated before they leave the pancreas. These enzymes are so powerful that they start to attack and digest the pancreatic tissue. This process is called autodigestion.
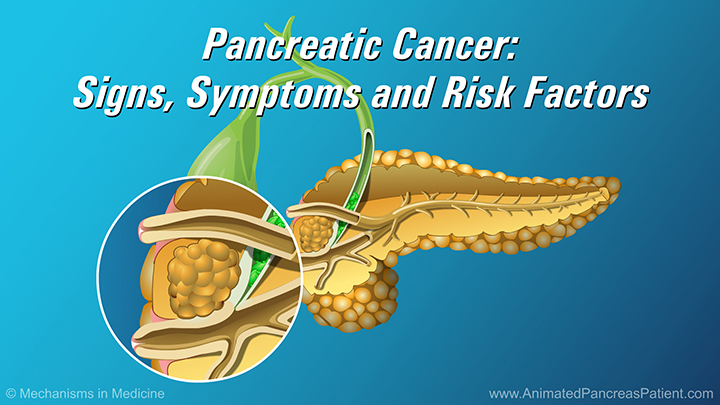
The most common causes of acute pancreatitis are heavy alcohol use and gallstones. Other less common causes include abdominal trauma, medications, infections, tumors, and genetic or anatomical variants. High triglycerides or high levels of calcium in the blood are also linked to acute pancreatitis. In some rare cases, the cause is never discovered.
Attacks of acute pancreatitis are usually sudden and characterized by intense pain in the center of the upper abdomen, between the belly button and the chest. The pain radiates to the back. Sometimes the pain can be on the left or right side, or even lower down in the belly.
Most people also have nausea and vomiting, and in some cases, fever.
Blood tests for pancreatic enzymes can diagnose acute pancreatitis. The pancreatic enzymes that typically are elevated when patients have acute pancreatitis are called the amylase and lipase.
Diagnosis is usually confirmed by a CT scan. On occasion MRI or ultrasound may be used. The radiologist will look to see if the pancreas is swollen or if there is abnormal fluid around it.
Most people who develop acute pancreatitis are out of the hospital in a few days.
However, about 1 in 10 cases are serious enough to affect other organs like the kidneys and lungs, and may require a longer stay in the hospital. Sometimes patients have to be treated in the intensive care unit.
In very severe cases, surgery may be required to remove inflamed parts of the pancreas. If the cause of acute pancreatitis was related to gallstones, the gallbladder is removed surgically. As well, in some patients, the pancreas becomes so damaged that it no longer functions properly to make digestive enzymes. This is called pancreatic insufficiency
Following an episode of acute pancreatitis, patients are advised to avoid alcohol and tobacco consumption, high fat foods and triglycerides, and medications that can put stress on the pancreas. As well, patients are encouraged to stay well-hydrated, and to eat a varied and healthy diet that is rich in fruits and vegetables.