Diagnosing Familial Chylomicronemia Syndrome (FCS)
*Please note: This slide show represents a visual interpretation and is not intended to provide, or substitute as, medical and/or clinical advice.
How is FCS diagnosed?
Doctors look for 3 things when diagnosing FCS.
One:
-
A blood test done on an empty stomach that shows triglyceride levels higher than 750 mg/dL, when other medical causes have been ruled out. Triglyceride levels are normally below 150 mg/dL.
How is FCS diagnosed?
Two:
- Little or no response to drugs that lower triglyceride levels.
How is FCS diagnosed?
And three:
-
A history of frequent episodes of abdominal pain or pancreatitis.
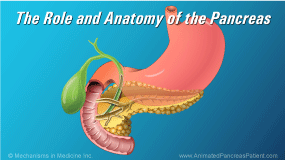
FCS leads to a high risk for acute pancreatitis
High levels of triglycerides are a common health problem, but very few people with high triglycerides––around eight in a million––have FCS. This small group of people is at high risk for recurrent episodes of acute pancreatitis, a painful complication of FCS.
Why is FCS hard to diagnose?
FCS is a rare condition that many doctors are not familiar with. As a result, patients with high triglyceride levels associated with recurrent bouts of pancreatitis may not be linked to FCS. In addition, symptoms of FCS may be mistaken for other diseases.
Unfortunately, there is no quick, simple test for FCS. Patients may have symptoms for many years before they get a correct diagnosis. Many patients are between 20 and 40 years of age when they learn that they have FCS although this can develop in children.
FCS and pregnancy
Women may be diagnosed with FCS after they become pregnant. If a woman has high triglycerides, being pregnant makes them rise further, and may lead to FCS being diagnosed.
Women with FCS who become pregnant face increased risks for pancreatitis, miscarriage, and other serious pregnancy complications.
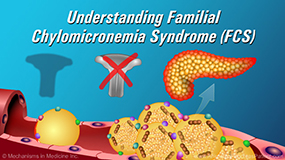
Gene changes associated with FCS
Some people with FCS have inherited two copies of an abnormal gene that disables an enzyme called lipoprotein lipase, or LPL. The body needs LPL to help it break down fat that is taken up by the intestine.
In about eight out of 10 people with FCS, this genetic abnormality occurs in the gene that activates LPL. Scientists have identified more than 100 different abnormal genes that cause LPL to not work properly.
What is genetic testing for FCS? - 1
A genetic test to establish a diagnosis of FCS requires the patient to provide a sample of saliva or blood for lab analysis. It may take a few weeks to get the results of the test. At this time, genetic testing for FCS is not routinely available outside of a research setting.
What is genetic testing for FCS? - 2
If you have FCS, your family members or relatives may also have it, or they may carry one copy of the abnormal gene.
People who have one abnormal gene are called carriers. They don’t have FCS, but if two carriers have a child together, there’s a one in four chance that the child will have FCS.
What challenges do people with FCS face? - 1
Living with FCS can be very stressful.
Researchers surveyed 166 people with FCS in 10 countries. About a third of them said that FCS “significantly interfered with their lives.”
What challenges do people with FCS face? - 1
The most common symptoms reported were abdominal pain, swelling or bloating in the abdomen, an upset stomach, and feeling weak or tired. Two thirds of these patients reported having pancreatitis.
What challenges do people with FCS face? - 2
People who took part in the survey also said that they worried about pain or an attack of pancreatitis, were anxious about their health, weren’t sure what they should eat or how much, and felt helpless because of FCS. Many people said that they worried about whether they should have children.
What challenges do people with FCS face? - 3
Many people who were not working or were working part time felt that having FCS had limited their work opportunities.
Talk to your doctor about FCS treatment options and follow a low-fat diet
If you have FCS, it’s important to talk with your doctor about your treatment options. It’s also very important to follow a diet that includes less than 20 grams of fat per day – that’s about 4½ teaspoons of olive oil per day. You can achieve this with help from your dietitian.
Talk to your doctor about clinical trials
At present there are no drug treatment options for FCS that have been approved by the FDA. However, new drugs for FCS are being tested in clinical trials.
Talk to your doctor about clinical trials
If you would like to find out more about clinical trials of new treatments for FCS, talk with your doctor or get in touch with the National Pancreas Foundation.
This slide show provides an overview of how
Familial Chylomicronemia Syndrome (
FCS) is diagnosed. Doctors look for 3 things when diagnosing FCS: a blood test to measure triglyceride levels, a patient’s response to drugs that lower triglyceride levels, and a history of frequent episodes of abdominal pain or pancreatitis. This slide show also describes the gene changes associated with FCS, genetic testing, the challenges of living with FCS, and clinical trials for new drug treatments.
-
Share with family and friends:
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about pancreatic diseases which will help other patients, caregivers and families.