Chronic Pancreatitis
*Please note: This slide set represents a visual interpretation and is not intended to provide, nor substitute as, medical and/or clinical advice.
Chronic pancreatitis is caused by long-term inflammation of the pancreas…
… which eventually leads to the irreversible destruction of pancreatic tissue.
Chronic pancreatitis develops slowly over time and is predominantly triggered by lifestyle factors in predisposed patients, such as long-standing, heavy alcohol or tobacco use. Although this is not always the case.
Other less common causes are medications that put stress on the pancreas; elevated triglycerides; some auto-immune conditions; and some inherited or genetic conditions, notably cystic fibrosis and hereditary pancreatitis. In some people, the cause of chronic pancreatis is never discovered and remains a mystery.
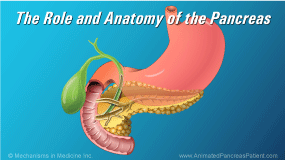
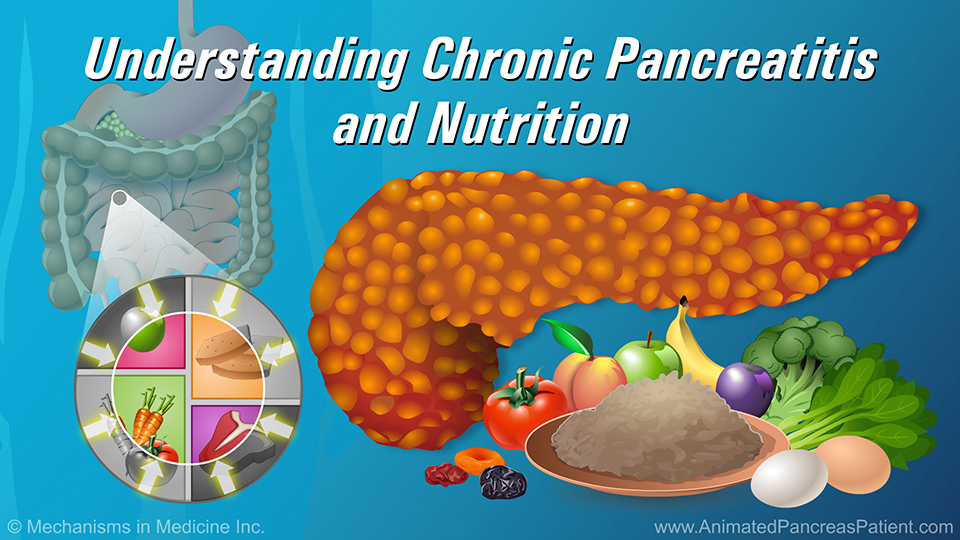
The pancreas is a digestive system organ that has two important functions. It produces hormones that regulate blood sugar, as well as enzymes to break down food in the digestive tract.
When the pancreas doesn’t work properly, it affects the body’s ability to properly digest food. This means that some people with chronic pancreatitis are unable to get the nutrients they need from the food they eat.
They can have trouble digesting food properly or maintaining their blood sugar in a healthy range.
This can lead to nutrition-related disease such as weak bones and vision loss. Some people may also have difficulty gaining or maintaining their weight, and persistent pain.
The hallmark symptom of chronic pancreatitis is abdominal pain. The pain may be intermittent or chronic, and frequently very severe, with stabbing pains localized in the upper part of the abdomen between the belly button and the chest. The pain may radiate to the back and may be triggered by eating, especially high-fat foods.
As the disease progresses, the pain may become more severe and debilitating, and often it becomes constant. In some cases, surgery or endoscopic treatment may be required.
Oily, foul-smelling bowel movements and weight loss may be seen in the advanced stages of the disease and usually signals exocrine pancreatic insufficiency. As well, depending on the severity and extent of the damage to the pancreas, some people develop diabetes.
A combination of tests are used to diagnose chronic pancreatitis. In some people, diagnosis is challenging due to the course of the disease; however in others it is relatively straight-forward.
A CT scan of the abdomen is the most commonly-used test. An MRI or endoscopic ultrasound may also be used to confirm the diagnosis.
In some difficult to diagnose cases, pancreatic stimulation testing can be useful. This test artificially stimulates the pancreas using secretin. This test is expensive and invasive, so it is not frequently performed.
Blood tests are not useful for diagnosing chronic pancreatitis.
Although there is no cure for chronic pancreatitis, early diagnosis and treatment can help slow the progression of the disease. Treatment involves avoiding triggers – such as heavy alcohol use, smoking, and high-fat foods.
Other treatment interventions involve pain management, medication, such as pancreatic enzyme replacement therapy (PERT), and supporting a healthy diet with multivitamin and mineral supplements.
This slide show describes the causes, symptoms, and factors in the development of chronic pancreatitis, as well as tools and tests used to diagnose the disease.
-
Share with family and friends:
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about pancreatic diseases which will help other patients, caregivers and families.