Understanding Endoscopic Retrograde Cholangiopancreatography (ERCP)
*Please note: This slide set represents a visual interpretation and is not intended to provide, nor substitute as, medical and/or clinical advice.
Endoscopy is a medical procedure in which a flexible instrument, that has a camera on the end, called an endoscope is passed into an area of the body, such as the gastrointestinal (GI) tract.
Physicians specializing in diseases of the digestive system are known as gastroenterologists.
Gastroenterologists use endoscopy to view the inside of a patient’s body, and may employ a variety of endoscopic procedures.
Depending on what is being examined, several other types of endoscopic procedures can be used.
Esophagogastroduodenoscopy (EGD) is used to examine the lining of the esophagus, stomach, and duodenum.
Enteroscopy is used to examine deeper into the small bowel, and is useful when other imaging techniques have shown an abnormal finding that can’t be reached using EGD or colonoscopy.
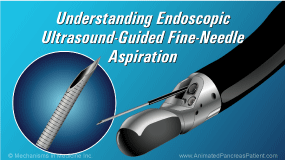
Endoscopic ultrasound (EUS) combines endoscopy with ultrasound to obtain images and tissue samples of the surrounding organs along the GI tract.
Endoscopic Retrograde Cholangiopancreatography (ERCP) is an endoscopic procedure used to examine and treat a specific finding within either the pancreatic duct or biliary tree (bile duct). This procedure helps your doctor make critical decisions concerning your health.
Once your doctor has taken a full medical history, established a treatment plan, and has determined that there is a need for ERCP, the risks, benefits and alternative treatments will be discussed with you.
You will be asked to sign an informed consent that acknowledges that you understand the risks and benefits of the procedure, and authorizes your doctor to proceed.
Preparing for ERCP is very important. The upper GI tract must be empty. No eating or drinking is allowed for 8 hours before ERCP. Medications may be restricted prior to and after ERCP. This will be determined by your doctor, with particular attention given to patients who have hypertension, diabetes, who take blood thinner medications, or who have bleeding disorders.
After the procedure, you will need a family member or a close friend to drive you home. Because of the medications used during the procedure, you should take the rest of the day off and you should not make any major decisions.
Your doctor will provide written instructions on how to prepare for your ERCP, the follow up care required at home, and how to recognize complications in case they occur.
ERCP is a therapeutic procedure performed in a patient with symptoms, abnormal findings by CT scan, MRI, ultrasound, or x-ray, together with abnormal lab results.
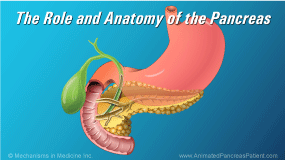
In the pancreatic duct, in an effort to relieve pain, ERCP is most commonly used to obtain tissue, remove stones, and drain fluid collections when symptoms are present.
Pain in chronic pancreatitis can be caused by pancreatic duct obstructions from stones, strictures, infections, or compression from fluid collection.
In the biliary tree, ERCP is frequently used to remove bile duct stones and to bypass obstructions that can be benign or malignant.
ERCP is also used to treat strictures, infections (such as cholangitis), leaks after surgery (such as gallbladder removal), and to obtain tissue samples in the form of biopsy or cytology.
ERCP is generally performed as an outpatient procedure, but on occasion it is performed when the patient is in the hospital for an acute problem.
Gastroenterologists may work alongside anesthesiologists to provide sedation.
A local anesthetic may be applied as a spray to your throat to numb the gag reflex. Your vital signs will be closely monitored throughout the procedure.
The procedure may be short or lengthy, depending on the complexity of the case.
A mouth piece will be used to protect both your teeth and the scope.
The ERCP scope is inserted into the mouth, passed through the esophagus, into the stomach and duodenum.
Air is insufflated to distend the duodenum and allow visualization. Once the scope is in the duodenum, the major papilla (also known as the Ampulla of Vater) is located.
It is important to note that secretions from both the pancreas and the bile duct jointly drain into the duodenum through the major papilla.
A guide wire and a catheter are inserted through the opening of the papilla to gain access to the pancreatic or bile duct – depending on where the disease lies.
The pancreatic duct is accessed via the major papilla and allows the endoscopic procedure to be carried out.
Using fluoroscopy (which is a combination of an X-ray machine, guide wire, and contrast dye injected via catheter) the desired duct is cannulated and the doctor is able to identify the problem and provide treatment.
If a stone is identified in either the pancreas or biliary tree, it can be removed by cutting the sphincter muscle within the major papilla – this is called a sphincterotomy.
The stone is removed by pulling it out of the duct and into the small bowel using a balloon to sweep and clean the duct. It can then pass out safely with the stool.
If a blockage or suspicious tissue is observed, a sample can be obtained and sent to the lab for analysis.
In the pancreatic duct, when fluid collection, stones, or strictures are present, a plastic stent can be inserted to bypass the obstruction or to drain the fluid. Once the obstruction is bypassed, the normal flow can be re-established.
In the bile duct, if a tumor causes blockage and requires drainage, a metal stent (if malignant disease) or plastic stent (if it is unknown if the obstruction is benign or malignant) can be used to bypass the blockage and re-establish the flow into the duodenum.
ERCP is more invasive than routine endoscopic procedures, and carries risks of complications, including acute pancreatitis in about 5 to 15% of cases, depending on the indication.
If pancreatitis occurs, hospitalization for a few days is usually required.
Other less common complications (particularly if sphincterotomy was performed) includes: Bleeding, infection, perforation, and possibly even death.
ERCP is an advanced endoscopic procedure that should be performed by well-trained and experienced physicians.
You should not hesitate to ask your doctor about how much experience they have performing ERCP. Your doctor is here to help you, and if necessary will refer you to a sub-specialist doctor.